New technique kills cancer cells within 3 days
Groundbreaking research appears to have identified cancer’s weak spot, which has led to the near-eradication of cancer in cell cultures within just a few days of application.
Altering the structure of chromatin in cancer cells could help to kill them, according to researchers at Northwestern University who published their study in the journal Nature Biomedical Engineering.
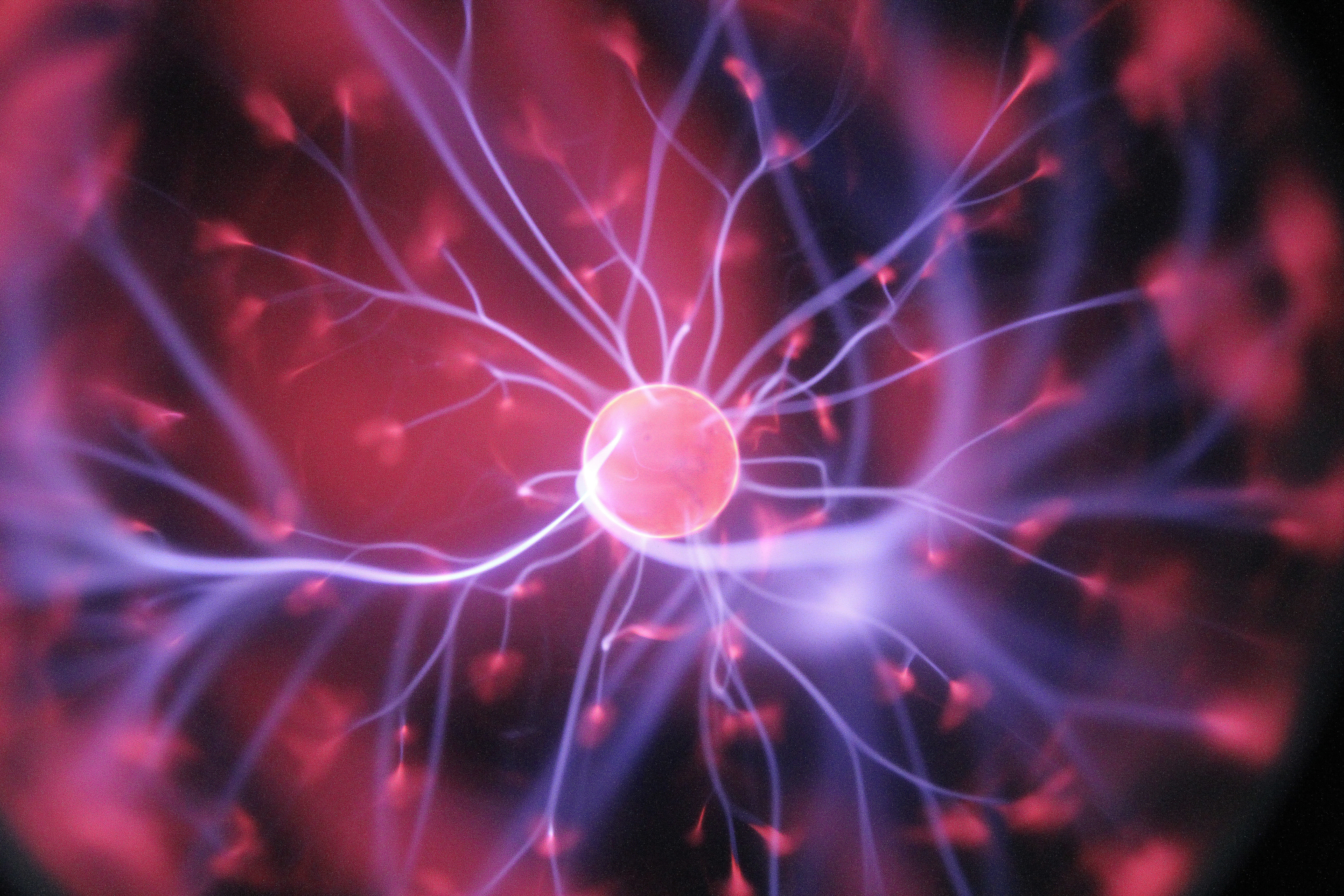
The study reveals how altering the structure of chromatin in cancer cells could make them easier to destroy. In the cell nucleus, DNA is wrapped around proteins called histones; combined, they form chromatin, reports Dr. Mark McKenna, a medical doctor and entrepreneur who regularly blogs about medical breakthroughs.
Chromatin serves to encapsulate the genetic code within the cell’s nucleus. Chromatin can also regulate which genes are switched on and off. In cancer cells, however, chromatin helps them to evolve and adapt to cancer therapies, thereby allowing them to survive.
The research team honed in on chromatin as the key to combating cancer drug resistance, and has developed an imaging technique to learn more about these macromolecules. The new technique is called Partial Wave Spectroscopic (PWS) microscopy, and it enables real-time monitoring of chromatin in living cells.
Researchers used PWS to monitor chromatin in cultured cancer cells, and found that chromatin has a specific “packing density” associated with gene expression that helps cancer cells to evade treatments, explains Dr. Mark McKenna.
New technique kills cancer cells within 3 days
The team found that they could modify chromatin’s structure by altering electrolytes in the nucleus of cancer cells. They tested this strategy using two drugs that are already approved by the Food and Drug Administration (FDA): Celecoxib and Digoxin. Both drugs are also able to change the packing density of chromatin.
The researchers combined these drugs — which they refer to as chromatin protection therapeutics (CPTs) — with chemotherapy and tested them on cancer cells in the laboratory. This revealed “something remarkable,” researchers say.
The scientists caution that animal and human studies are needed before any firm conclusions can be made. However, they have replicated their findings in seven different cancer types so far, and the results are “very promising.”
Replica of blood-brain-barrier could lead to drug discoveries
Scientists have devised a method to create an exact laboratory replica of the human blood-brain barrier. This development will open doors to new research on the properties of these barrier cells, so scientists can uncover new therapies that bypass the barrier, reports Dr. Mark McKenna.
The barrier is the brain’s first line of protection, but the barrier is a frustrating-yet-effective block to many small-molecule drugs that might provide effective therapies for neurological conditions, including cancer, stroke, and trauma.
In their report published in Science Advances, researchers from the University of Wisconsin-Madison detail a defined, step-by-step process that uses small molecules to guide cells through the developmental process. The method substitutes chemical factors for cells to push stem cells to become the brain endothelial cells that compose the blood-brain-barrier.
Stem cell science has been described as an art and a science, as it involves directing stem cells to become any of the hundreds of cell types that make up the human body, explains Dr. Mark McKenna.
By identifying specific chemical molecules that can usher the cells through development stages to become the brain endothelial cells, the research team provides a recipe to standardize making the cells in quantities useful for research.
Using adult cells from patients, which are reprogrammed to an embryonic stem cell-like state, will allow researchers to better understand the etiology of neurological disorders, including brain infections and multiple sclerosis.
This development standardizes the research approach, which can be applied to a wide variety of cells. Scientists will be able to track cells as they progress through various phases – which will help clarify the cellular events that occur as neurological conditions develop.
With this new method, pharmaceutical companies will be able to scale up production of the brain endothelial cells for drug discovery. By exposing cells to various agents, researchers can assess toxicity and effect of promising therapies.
Influenza virus may have a new enemy
As flu season sets in, researchers from the University of Colorado Boulder and University of Texas at Austin have published a study revealing a previously unknown mechanism by which the human immune system tries to battle the influenza A virus. Their paper appeared in the Nov. 8 issue of Cell Host and Microbe.
The discovery sheds new light on how the virus — which kills up to 56,000 people in the United States annually — often wins, and it could lead to new treatments. Scientists anticipate it will lead to a better understanding of how the seasonal flu virus, which typically originates in birds, makes its way to humans.
Researchers also expect this will lead to next-generation antivirals able to combat a broad spectrum of influenza strains, reports Dr. Mark McKenna.
The paper outlines two key molecular players involved in influenza infection: a human protein called TRIM25, which plays an important role in the human immune response to flu infection; and a protein called NS1 present in all strains of the influenza A virus – and binds with TRIM25 to keep it from doing its flu-fighting job.
Previous research suggested that TRIM25 fought off flu by switching on what is known as the “interferon response” — a complex signaling pathway that arms cells through the body to fight off pathogens. But not all strains of influenza block this interferon signaling pathway, which led researchers to suspect another mechanism was at play in helping TRIM25 fight flu.
The paper reveals that TRIM25 is also a “restriction factor,” a special protein present in the fastest-acting arm of the immune system, before spreading infection occurs, explains Dr. Mark McKenna. Restriction factors wait for a virus to be detected in a cell, and have immediate destructive ability. Flu uses its NS1 protein to evade TRIM25’s early flu-fighting response, the researchers found.
Researchers believe new therapeutics could block the NS1 protein produced by the flu virus, short-circuiting its ability to evade the human immune system.
About Dr. Mark McKenna:

- Mark McKenna, MD, MBA is a Medical Doctor licensed in Surgery and Medicine by the Georgia and Florida State Board of Medical Examiners. He is a passionate patient advocate and a dedicated community servant.
Dr. McKenna was a featured guest on the inaugural episode of a CBS television show entitled Doctorpreneur which highlighted the entrepreneurial spirit in the medical and healthcare communities.
A native of New Orleans, he has previously served as a board member of the New Orleans Jazz Festival and the New Orleans Industrial Development Board.
Source:
https://www.sciencedaily.com/releases/2017/11/171108151614.htm














Leave a Reply
Be the First to Comment!
You must be logged in to post a comment.
You must be logged in to post a comment.